Integrating Mental Health into NCD Care in Primary Care
A WONCA Advocacy Project
By Dr. Stephen T. Engmann
This project was born out of a deepening concern for the burden of mental health issues among patients living with non-communicable diseases (NCDs) in Ghana. In our urban primary care setting, at the Manna Mission Hospital in Accra, a needs assessment was conducted to evaluate the burden of common mental health issues among patients with hypertension and type 2 diabetes mellitus. Recognizing the gap, Dr. Stephen T. Engmann led a practice quality improvement project to bridge the divide between physical and mental health care in primary care delivery.
The catalyst for this initiative was the World Organization of Family Doctors (WONCA), under its Integrating Care Leadership and Advocacy Programme. This programme was specifically designed to empower young family physicians to lead innovations in integrating behavioural and physical health. In collaboration with the Farley Health Policy Centre (FHPC), Columbia University, the WONCA Working Party on Mental Health, and the WONCA Young Doctors Movement (YDM), the programme ran for nine months from August 2023. Participants were paired with senior mentors from the WONCA Mental Health Working Group and tasked with conceptualizing and executing integrated care projects in their local contexts.
Under this framework, Dr. Engmann’s team initiated the project between September 2023 and April 2024. The project activities were thoughtfully designed to raise awareness, empower healthcare providers, and implement pragmatic screening for mental health within NCD care. Key interventions included:
Educational posters in English and local languages (Ga and Twi) were displayed in waiting areas and consultation rooms to highlight common warning signs of mental health issues and sources of help.
 Figure 1: Educational poster
Figure 1: Educational poster
Routine screening was introduced using the PHQ-4 tool for patients aged 18 and older with hypertension or type 2 diabetes. This screening was incorporated into standard consultations from October 2023 to January 2024.
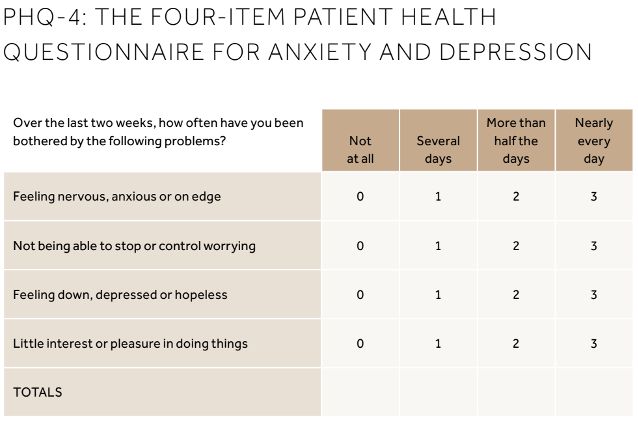 Figure 2: PHQ-4 tool (Kroenke K, Spitzer RL, Williams JB, Löwe B. An ultra-brief screening scale for anxiety and depression: the PHQ-4. Psychosomatics. 2009;50(6):613-21.)
Figure 2: PHQ-4 tool (Kroenke K, Spitzer RL, Williams JB, Löwe B. An ultra-brief screening scale for anxiety and depression: the PHQ-4. Psychosomatics. 2009;50(6):613-21.)
Health talks were organized in October, January, and April across outpatient and chronic care clinics to demystify mental health and promote help-seeking behaviour.
 Figure 3: Health Talk
Figure 3: Health Talk
Clinical meetings focused on the biopsychosocial model of care, and self-care of the healthcare provider were held twice during the duration of the project. These sessions were instrumental in generating buy-in from the broader primary care team.

Figure 4: Clinical Meeting
The project screened 205 adult patients, uncovering that 21% screened positive for probable anxiety or depression. Upon further evaluation, 39 patients (19%) were diagnosed with either or both conditions, ranging from mild to severe depression and generalized anxiety disorder. Treatment involved both pharmacological and non-pharmacological options, including cognitive behavioural therapy depending on severity. Notably, 36 of those patients saw symptom resolution within six months of intervention.
Beyond the numbers, the project catalyzed a culture shift within the primary care facility. Mental health, often relegated to the sidelines, gained prominence within chronic disease management. Providers were more confident in recognizing psychological distress, patients felt seen and heard, and care became more holistic. However, the project was not without challenges. Language barriers occasionally hampered accurate screening and added responsibilities slightly increased doctors’ workloads. Nonetheless, opportunities exist for scaling the model to other chronic conditions and expanding training in integrated care across the healthcare workforce.
The project supports the argument that mental health integration into NCD care is both feasible and impactful, especially in low-resource primary care settings. This model enhances patient outcomes, reduces treatment fragmentation, fosters holistic care, and contributes to destigmatizing mental health concerns.
For the full report, see the article published in the African Journal of Primary Health Care & Family Medicine: https://doi.org/10.4102/phcfm.v17i1.4875