International PHC and COVID-19 Study
Prof Felicity Goodyear-Smith reports on the recent research that has been done through WONCA networks. The research team is Felicity Goodyear-Smith, Karen Kinder, Robert Phillips, Andrew Bazemore, Cristina Mannie, and Stefan Strydom
Aim:
This multinational survey aimed to understand characteristics and strategies employed by different countries to deal with COVID-19 from a PHC perspective to determine:
• Factors most associated with national mortality rates during the pandemic period to date
• Lessons to better address both current and future pandemics
Preliminary Results
(1035 responses, 111 nations):
What factors correlated most with lower death rates?
• Testing: Lower death rates were observed in countries where participants indicated that the following testing practices were employed:
o Having readily available testing at the time of first COVID death
o Testing all incoming travelers
o Testing symptomatic persons
o Testing those exposed to COVID positive individuals
• Movement Restrictions: Lower death rates were observed in where participants indicated that the following testing practices were employed:
o Physical distancing
o Event closures
o Closure of all but essential services
o Isolation based on contact tracing
o Self-Isolation in households
o Quarantine for suspected cases
Strong PHC System and Death Rates: Existing strong PHC systems were not correlated with death rates. This may be attributed to:
• Uncoordinated responses between public health and PC personnel
• Lack of PPE and testing for community-based workers
• Irrelevance of PHC if potential carriers were stopped at the border (most relevant to small island nations)
• PC not being engaged
Methods:
1131 surveys were collected from PHC clinicians (73.0%), researchers (16.9%), and policymakers (10.0%) across the world. The survey was distributed in both English and Spanish via PHC networks and snowballing. Participants were asked a series of questions that addressed the nature of their PHC system, how it responded to the pandemic, the use of health information technology in their country, if their country had a pandemic plan, and various strategies utilized to respond to the virus. Countries that had 10 or more surveys are referred to as the “top 21 countries”.
 Data for Each Country:
Data for Each Country:
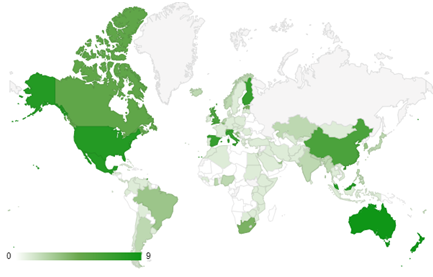
For each country, the maximum death rate on a 7-day moving average served as the response variable in the survey. Map shows the distribution of respondents.
Analyses:
Univariate, bivariate, regression model analyses, and thematic analysis were employed to arrive at the preliminary results.
Current Public Health and Primary Care Responses:
• Hygiene Measures: hand washing and wearing PPE
•
Limit person-to-person contact: physical distancing, ban mass
gatherings, primary care provided remotely, self-isolation, and shutdown
• Identify Cases: testing, contact tracing, and surveillance
Current Approaches to Address the Pandemic:
Most countries utilized a combination of the following strategies:
• Blocking entry to country: border control, testing and or quarantining new arrivals
• Reducing the spread within the country: employing a variety of public health and primary care measures
• Managing severe cases to reduce deaths: hospitalization, oxygenation, ventilation, and intensive care
“Primary health care perceptions of COVID-19 responses on rate of death: an international study”, Felicity Goodyear-Smith, Karen Kinder, Andrew Bazemore Robert Phillips, Stefan Strydom, Cristina Mannie, under consideration for publication, 2020. For further information, please contact Andrew Bazemore at
abazemore@theabfm.org