WP on Mental Health: Advocacy is an art that can be learned
 Christopher Dowrick, WONCA Working Party for Mental Health
Christopher Dowrick, WONCA Working Party for Mental Health
This program was funded by a discretionary grant from WONCA Executive, the Farley Center and faculty volunteerism.
Background
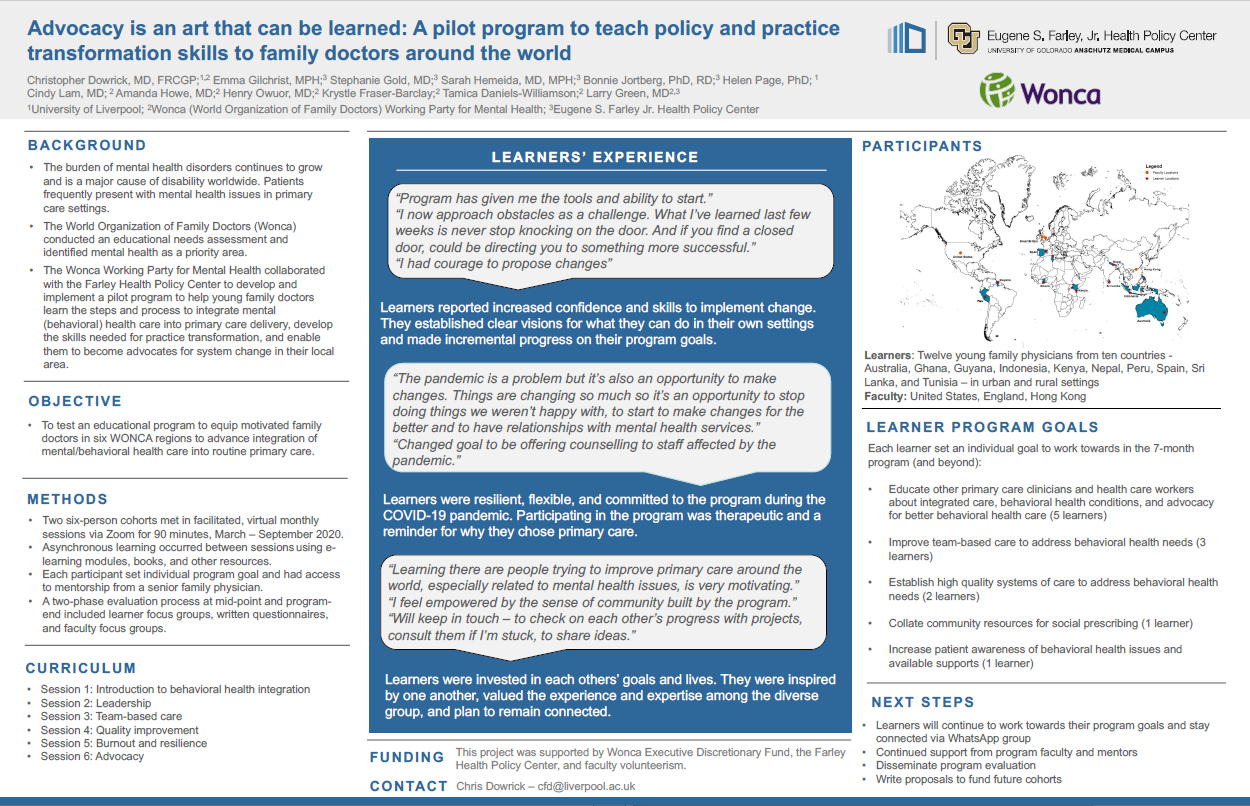
The burden of mental health disorders continues to grow and is a major cause of disability worldwide. Patients frequently present with mental health issues in primary care settings. The WONCA Working Party for Mental Health collaborated with the Farley Health Policy Center to develop and implement a pilot program to help young family doctors learn the steps and process to integrate mental health care into primary care delivery, develop the skills needed for practice transformation, and enable them to become advocates for system change in their local area.
Methods
Learners: Twelve young family physicians from ten countries - Australia, Ghana, Guyana, Indonesia, Kenya, Nepal, Peru, Spain, Sri Lanka, and Tunisia – in urban and rural settings.
Faculty: United States, England, Hong Kong
Two six-person cohorts met in facilitated, virtual monthly sessions via Zoom for 90 minutes, March – September 2020. Asynchronous learning occurred between sessions using e-learning modules, books, and other resources. Each participant set individual program goal and had access to mentorship from a senior family physician. A two-phase evaluation process at mid-point and program-end included learner focus groups, written questionnaires, and faculty focus groups.
Curriculum
• Introduction to behavioral health integration
• Leadership
• Team-based care
• Quality improvement
• Burnout and resilience
• Advocacy
Learner Program Goals
• Educate other primary care clinicians and health care workers about integrated care, behavioral health conditions, and advocacy for better behavioral health care (5 learners)
• Improve team-based care to address behavioral health needs (3 learners)
• Establish high quality systems of care to address behavioral health needs (2 learners)
• Collate community resources for social prescribing (1 learner)
• Increase patient awareness of behavioral health issues and available supports (1 learner)
Evaluation
• Learners reported increased confidence and skills to implement change. They established clear visions for what they can do in their own settings and made incremental progress on their program goals. “I now approach obstacles as a challenge. What I’ve learned last few weeks is never stop knocking on the door. And if you find a closed door, could be directing you to something more successful.”
• Learners were resilient, flexible, and committed to the program during the COVID-19 pandemic. Participating in the program was therapeutic and a reminder for why they chose primary care.
• Learners were invested in each other’s goals and lives. They were inspired by one another, valued the experience and expertise among the diverse group, and plan to remain connected. “Learning there are people trying to improve primary care around the world, especially related to mental health issues, is very motivating.”
Next Steps
• Learners continue to work towards their program goals and stay connected via WhatsApp group, and with support from program faculty and mentors.
• Write proposals to fund future cohorts.
 Read the complete article - Advocacy training for young family doctors in primary mental health care: a report and global call to action
Read the complete article - Advocacy training for young family doctors in primary mental health care: a report and global call to action