World Patient Safety Day: Improving Diagnosis for Patient Safety

World Patient Safety Day
17 September 2024
Prof Maria Pilar Asteria-Peña
On September 17, World Patient Safety Day will be celebrated, an event that since 2019 has been part of the World Health Organization (WHO)’s public health campaigns.
With the theme "Improving Diagnosis for Patient Safety" and the slogan "Right Diagnosis Safe Patients!" World Patient Safety Day 2024 highlights the importance of accurate and timely diagnosis for patient safety.
Although diagnostic errors — along with issues related to medication use — have some of the worst consequences for patients and professionals, they have not been the focus of attention until 2015 when the report "Improving Diagnosis in Health Care" was published.
In its announcement of World Patient Safety Day 2024, the WHO describes diagnostic error as a situation where the patient's health problem is not correctly or timely explained. This includes the absence of a diagnosis, incorrect diagnoses, delays in diagnosis, and failures to communicate the diagnosis. The UN health agency highlights that diagnostic errors account for almost 16% of preventable harm in healthcare systems and estimates that most adults will face at least one diagnostic error in their lifetime.

Sharing experiences and thoughts from family medicine with Dr Albert Wu
The campaign website details the objectives, key messages, and practical advice for improving the diagnostic process aimed at different stakeholders (patients and their families, healthcare workers, health sector leaders, policymakers, and civil society). In the "Logos and Campaign Materials" section, after accepting the terms of use, the graphic materials for promoting the campaign can be downloaded. Logos and communication assets (posters, infographics, web and social media banners, wallpapers, etc.) are available in the six UN languages (English, Arabic, Chinese, French, Spanish, and Russian).
Additionally, as in previous years, and to boost global campaign awareness, the WHO is encouraging the 194 Member States to light up work centers, iconic monuments, or well-known sites in orange, urging them to organize specific activities around September 17 and to share the initiatives developed. The information collected (in English) will be used as a basis for evaluating the campaign and may appear in the report that WHO will prepare on the initiatives carried out for World Patient Safety Day 2024.
Materials prepared by the World Health Organization for the celebration of World Patient Safety Day 2024
The WHO notes that to improve the safety of the diagnostic process, action is needed on both systemic and cognitive factors. Systemic factors involve organizational shortcomings that predispose to errors, such as poor communication between healthcare staff or between staff and patients, work overload, and deficiencies in teamwork. Cognitive factors relate to the training and experience of professionals, their predisposition to cognitive biases, and other factors that increase the risk of human error in healthcare, such as fatigue and stress.
It is noteworthy that most diagnostic errors related to cognitive biases are not due to a lack of knowledge but to failures in gathering, verifying, integrating, and interpreting information.

.

Therefore, for family doctors, keeping information in the medical record up-to-date is essential for tailoring interventions to the patient's characteristics. The electronic health record allows all of a patient's health information to be included in a single support system regardless of where and when it is generated. A traceability of information that was previously unthinkable with paper records.
On the flip side, if the information is not reviewed, organized, and updated, medical records can become a maze of disconnected data that complicates decision-making and increases the risk of inappropriate interventions. It is crucial to eliminate inappropriate, erroneous, or outdated diagnoses from the medical record. This contributes to patient safety, just as regularly reviewing and adjusting pharmacological treatments does.
A delayed or incorrect diagnosis, or the absence of a diagnosis, generally leads to a worse prognosis, can prolong illness, and sometimes cause disability or even premature death. Failures in the diagnostic process are accompanied by delays in starting appropriate treatment and can lead to providing the patient with unnecessary or harmful treatment, which also has psychological and economic repercussions.

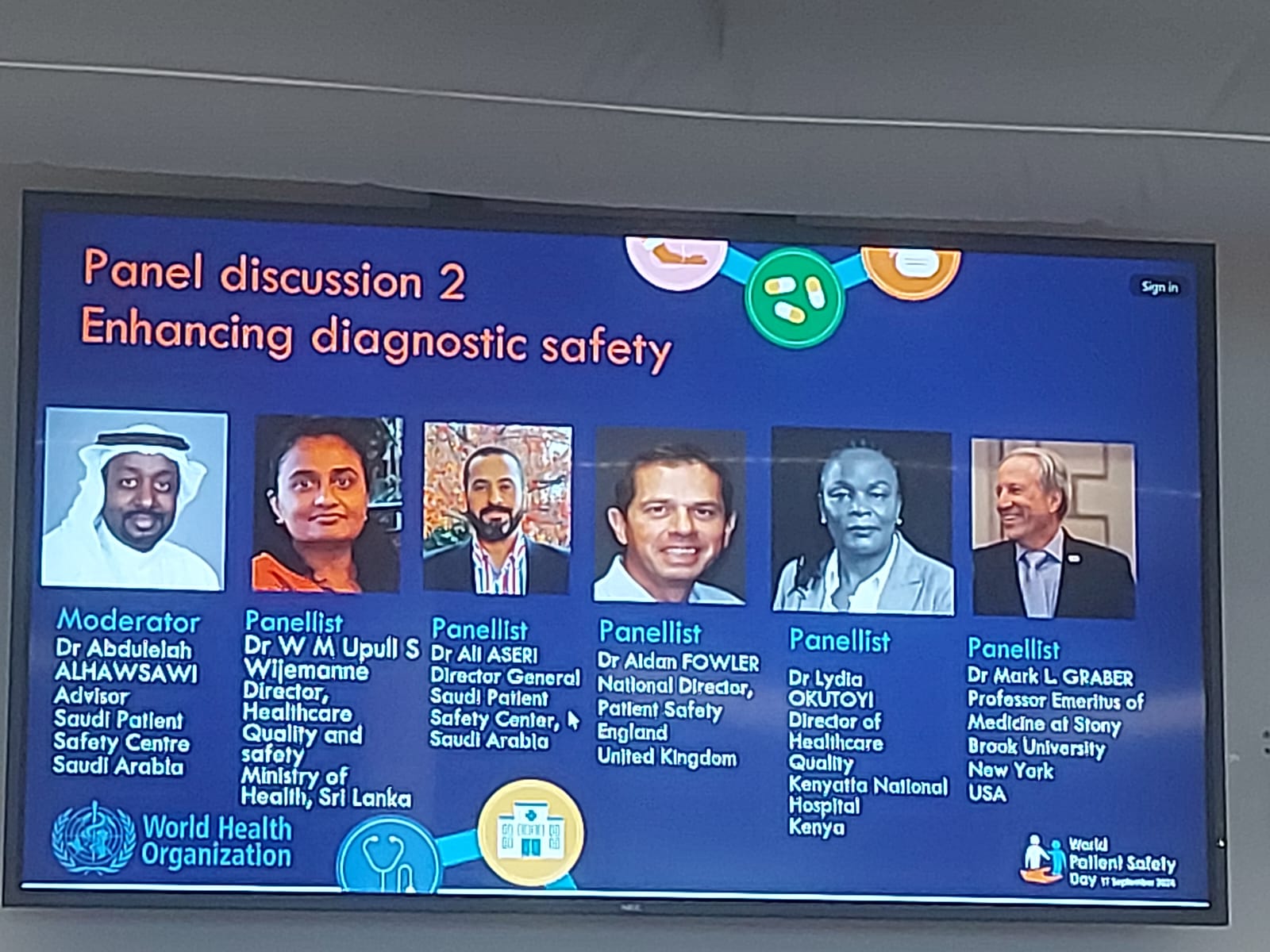
Building a safe diagnosis with team perspective. Annagret Hannawa, Wolf Hautz, Laura Zwart, Mark Graber, Hardeep Sighn, with WONCA representative Prof Maria Pilar Asteria-Peña
The role of family doctors in the safe diagnosis process
Family doctors play a critical role in ensuring a safer diagnosis process in primary care. Their contributions to patient safety in diagnosis include the following key areas:
1. Comprehensive healthcare
Family doctors often have a long-term relationship with patients, allowing them to understand the patient’s medical history, lifestyle, and psychosocial factors. This deep understanding enables more accurate clinical judgments and timely diagnosis as they can consider the full context of a patient's health. For example, knowing a patient's family history of heart disease, a family doctor might promptly recognize subtle symptoms of cardiovascular issues, leading to earlier diagnosis and intervention.
2. Early detection and prevention
Family doctors serve as the first point of contact for patients, making them essential in detecting early signs of disease. By performing routine screenings and physical exams, they can identify risk factors and symptoms that might otherwise go unnoticed. For example, implementation of regular screening programas such as colon cancer or blood pressure checks in patients at risk of hypertension and cardiovascular diseases help prevent serious complications.
3. Continuity of Care and Monitoring
Family doctors provide continuous care, which allows for the tracking of symptoms over time. This helps in diagnosing conditions that evolve slowly or present with ambiguous symptoms. Continuity also aids in adjusting treatment plans when conditions change or new information arises. For example: In chronic conditions like diabetes, family doctors monitor long-term health changes and ensure timely adjustments in treatment plans to avoid complications.
4. Comprehensive Physical and Mental Health Assessments
Family doctors are trained to assess both physical and mental health, which is crucial as many conditions have overlapping or psychosomatic symptoms. This comprehensive approach helps prevent diagnostic errors, such as misdiagnosing depression for fatigue or vice versa. For example, recognizing that a patient's physical symptoms (e.g., fatigue, headaches) might be linked to underlying depression or anxiety, the family doctor can avoid unnecessary medical interventions and provide appropriate mental health care.
5. Patient Communication and Shared Decision-Making
Family doctors often have well-established relationships with their patients, fostering better communication. Clear explanations and discussions of symptoms, treatment options, and diagnostic tests reduce misunderstanding and ensure patients are active participants in their care. For example, a family doctor explains the pros and cons of various diagnostic tests (e.g., MRI, CT scan) and involves the patient in deciding the most appropriate steps, ensuring that diagnostic tests are both necessary and understood.
6. Coordinating with Specialists
When conditions require specialist referral, family doctors play a key role in referring patients, providing essential background information, and coordinating care. This helps ensure that specialists receive a clear picture of the patient’s health, reducing the risk of fragmented care and diagnostic errors. For example, a family doctor identifies potential early signs of cancer and coordinates with an oncologist, sharing detailed medical history and test results for more accurate diagnosis and treatment planning.
7. Error Prevention through Diagnostic Stewardship
By avoiding over-testing or unnecessary interventions, family doctors help prevent overdiagnosis and unnecessary treatments that can harm patients. They use clinical judgment to determine which tests and procedures are truly necessary. For example, a family doctor may avoid ordering an unnecessary MRI for a patient with back pain when conservative management is sufficient, preventing the patient from exposure to potentially invasive procedures.
8. Addressing Cognitive Biases
Family doctors are trained to recognize and mitigate cognitive biases (e.g., confirmation bias or anchoring bias) that could affect diagnostic decisions. By using evidence-based practices and actively questioning their own diagnostic reasoning, they improve the accuracy of diagnoses. For example, if a patient presents with recurrent headaches, the family doctor resists prematurely diagnosing it as a migraine, carefully considering other potential causes, such as neurological issues.
9. Fostering a Safe Environment for Open Communication
Family doctors create an environment where patients feel comfortable discussing symptoms, concerns, and even uncertainties. This encourages patients to share important but potentially overlooked information, which can be critical in making the right diagnosis. For example, patient might feel comfortable sharing subtle or embarrassing symptoms (e.g., changes in bowel habits), allowing the family doctor to investigate potential underlying conditions like gastrointestinal disorders.

.

In summary, family doctors contribute to safer diagnostic processes by combining their clinical expertise, patient-centered care, and preventive approaches. Their ability to build trust, ensure continuity, and balance clinical judgment with patient input makes them a vital part of the effort to reduce diagnostic errors in primary care.