MDD Minds for Primary Care. First meeting of the Master Faculty.
Today we had the first meeting to onboard the Master Faculty of the MDD Minds project, who will guide the curriculum and the content design, development, and implementation.
The members of the Master Faculty are specialists in Primary Mental Health Care and understand the particularities and challenges of the region where they practice.
The MDD Minds for Primary Care Project will require the development of a core curriculum and its adaptation to the different geographical regions where it will be implemented.
We were pleased to have experts from 9 countries who will provide their mentorship along this important journey.
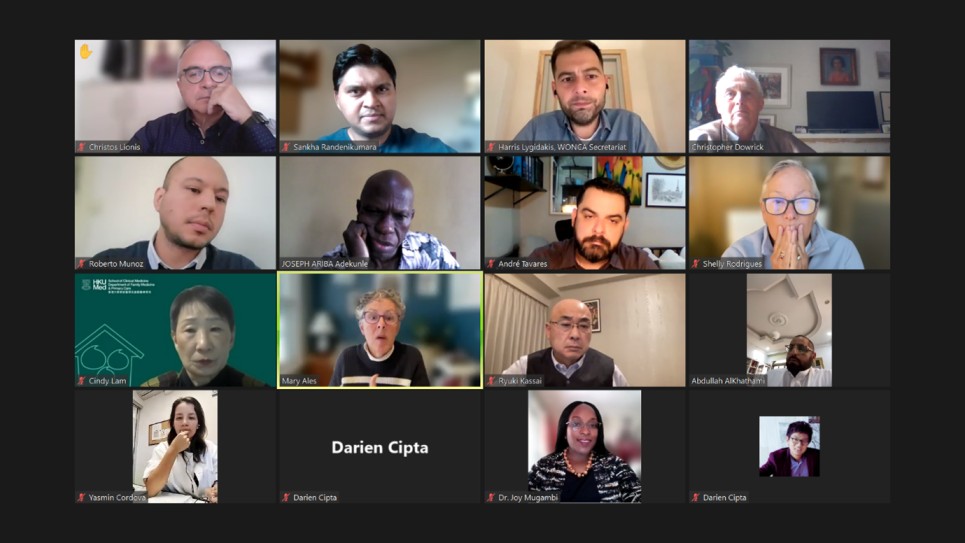
Joined the meeting, specialist from Brazil, Greece, Hong Kong, Indonesia, Japan, Kenya, Nigeria, Peru, Saudi Arabia, Sri-Lanka, United Kingdom, and United States.
Their involvement in the project is crucial to generate quality content that will make it possible to reach the goals of the project of improving the quality of care for patients suffering from major depressive disorders in Africa-Middle East, Asia Pacific, and Latin America.
MDD Minds for Primary Care | FAQS
Q. What is MDD Minds?
MDD stands for Major Depressive Disorder. WONCA is implementing MDD Minds for Primary Care Project, a 30-month project, in collaboration with the WONCA Working Party on Mental Health, and Mosaica Solutions.
Q. What is the goal of the project?
The overall goal of this program is to enhance the quality of care for major depressive disorders delivered by family doctors in Africa/Middle East, Asia, and Latin America.
Q. Why is it important?
Depression is a global issue, as it is now the leading cause of disability worldwide. Unfortunately, between 50% and 90% of people suffering from depression are not diagnosed or treated properly. The integration of mental health care into primary care, particularly within the field of family medicine, is a priority for international agencies.
The MDD Minds Project aims to strengthen physicians’ competencies and confidence in managing mental health problems while enabling shared decision-making for treating major depressive disorders.
Q. Who are the beneficiaries of the project?
The ultimate beneficiaries are the patients. Their family doctor will acquire knowledge, develop skills, and be empowered in the diagnosis and management of MDD.
Q. How do you plan to achieve the goal?
By implementing a training course together with a train-the-trainer program and a performance in practice scheme to apply the acquired knowledge and skills.
The training is aimed to increase physician competence in identifying depression and anxiety, educating patients, and employing shared decision-making, selecting appropriate pharmacologic and non-pharmacologic therapy, communicating with specialists in making referrals, and follow-up with patients to revaluate care.
Because of this, the trained physicians will be better equipped to help patients suffering from depression and anxiety.
Q. How is the project funded?
The funds come from an unrestricted educational grant from Pfizer.
Q. Has the donor any influence on the project?
No, the main characteristic of an unrestricted grant is that the donor, in this case Pfizer, cannot influence any part or stage of the project (including its design, development, implementation, monitoring and dissemination phases), thus always guaranteeing its complete independency and autonomy.